AI in Medicine
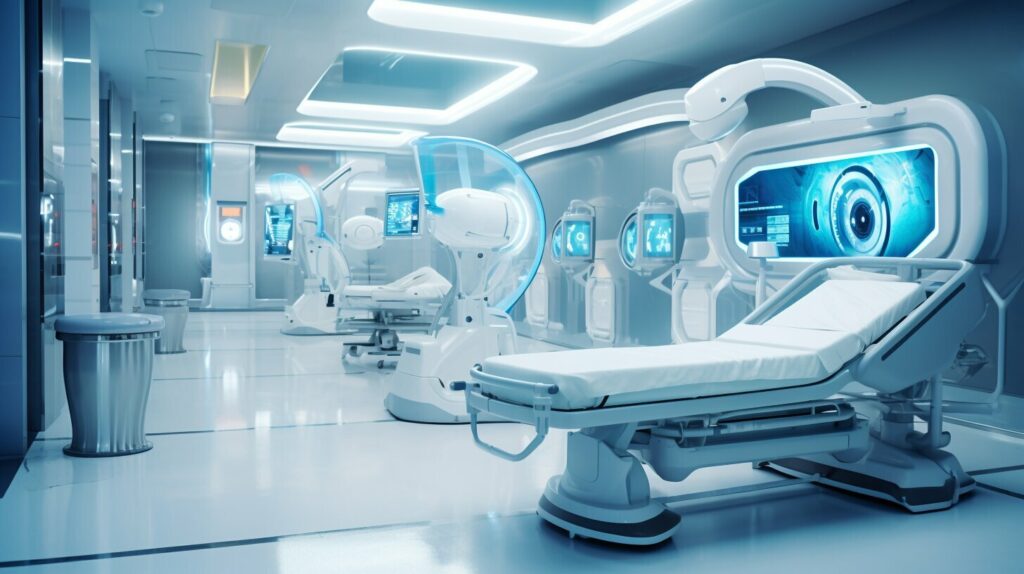
Revolutionizing Medicine: AI Solutions for Healthcare

Incorporating artificial intelligence (AI) into the healthcare sector represents a significant progress that promises to elevate the quality of patient care and propel medical research forward. The capabilities of AI technology extend to enhancing health literacy, empowering patients, and facilitating the management of chronic illnesses. Through AI’s application, healthcare practitioners are able to assemble dependable and enlightening videos for patients, construct engaging game-based platforms for children’s health education, and develop impartial models for assessing risks. This advent of AI solutions is radically changing the landscape of the healthcare field and evolving the practice of medicine.
Key Takeaways:
- AI technology in healthcare can improve health literacy and empower patients.
- Gamified platforms using AI can enhance pediatric health literacy.
- Unbiased risk assessment models powered by AI can assist in chronic disease management.
- AI solutions are revolutionizing the healthcare industry.
- AI can transform the way medicine is practiced.
Enhancing Health Literacy through AI
AI technology is transforming the healthcare landscape, offering innovative solutions to enhance health literacy and empower patients. By leveraging AI in healthcare, we can develop digital tools and platforms that provide accurate and understandable health information to patients. One example is digital therapeutics, where AI-powered software supports patients in making behavior changes to improve their health outcomes. With the help of natural language processing, AI can curate reliable and informative videos on various health topics, ensuring that the content is unbiased and easily comprehensible.
Healthcare providers can utilize AI technology to improve patients’ knowledge and understanding of their conditions, enabling them to make informed decisions about their care. By leveraging AI-driven algorithms, healthcare professionals can develop personalized risk assessment models that can accurately predict disease risks by analyzing comprehensive patient data. This allows for proactive interventions and tailored treatment plans, ultimately improving chronic disease management.
Furthermore, AI is revolutionizing pediatric health literacy through the development of gamified platforms. These platforms incorporate AI-enabled immersive gaming experiences that promote neurocognitive training and implicit learning. By engaging children in interactive and educational games, we can teach them about early childhood nutrition, physical activity, health-hygiene promotion, mental health, and overall wellness care. Ongoing research and randomized controlled trials are evaluating the effectiveness of these AI-based solutions in improving behavioral and clinical outcomes.
In summary, AI is playing a pivotal role in enhancing health literacy by providing reliable, accessible, and personalized information to patients. Through AI-powered digital therapeutics, risk assessment models, and gamified platforms, patients can gain a better understanding of their health conditions and make informed decisions about their care. As AI technology continues to advance, we have the opportunity to transform healthcare delivery and empower patients to take control of their well-being.
Digital Vaccines for Pediatric Health Literacy
AI and gamification are transforming pediatric health literacy through the development of innovative digital solutions. These mobile health gamified platforms, often referred to as “digital vaccines,” utilize artificial intelligence to incorporate neurocognitive training and implicit learning. By leveraging immersive gaming experiences, these digital vaccines aim to improve children’s knowledge about various aspects of health and wellness, including early childhood nutrition, physical activity, health-hygiene promotion, mental health, and wellness care.
Through ongoing research and randomized controlled trials, the effectiveness of these AI-based solutions in improving behavioral and clinical outcomes is being evaluated. By engaging children in a digital environment that is both educational and entertaining, these platforms seek to orient the brain toward healthy behaviors, promoting disease prevention and overall well-being.
A comprehensive approach to pediatric health literacy, these digital vaccines emphasize the importance of early education and engagement in health and wellness. By utilizing AI technology and gamification, healthcare providers can empower children to take an active role in managing their own health, equipping them with the knowledge and skills necessary for a lifetime of well-being.
| Platform Features | Benefits |
|---|---|
| Neurocognitive training through games | Enhances cognitive abilities and problem-solving skills |
| Interactive and engaging content | Increases children’s interest and motivation to learn about health |
| Personalized feedback and progress tracking | Allows parents and healthcare providers to monitor and support children’s learning |
| Evidence-based information | Ensures accuracy and reliability of health-related content |
These digital vaccines for pediatric health literacy are just one example of how AI is revolutionizing the healthcare industry. By leveraging technology and innovative approaches, we can empower the next generation to make informed choices about their health and well-being, ultimately leading to healthier communities and a brighter future.
AI for Improved Chronic Disease Management
Chronic diseases pose a significant burden on individuals and healthcare systems worldwide. However, the integration of artificial intelligence (AI) in healthcare offers promising solutions for improved chronic disease management. By harnessing the power of AI, healthcare providers can identify high-risk patients and tailor interventions accordingly, leading to more effective disease prevention and management strategies.
One of the key applications of AI in chronic disease management is the development of risk assessment models. These models leverage AI algorithms to analyze large quantities of comprehensive data, including patient demographics, medical history, lifestyle factors, and biomarkers. By identifying patterns and correlations within this data, AI algorithms can accurately predict disease risks, allowing healthcare providers to intervene early and provide personalized care.
However, it is crucial to develop unbiased and equitable risk assessment models to ensure fair and effective healthcare solutions. AI algorithms must be designed to address potential biases in the data and consider diverse populations. This requires asking the right questions and addressing any potential blind spots in the data collection and analysis process. Only by doing so can we create AI models that provide accurate and reliable tools for chronic disease monitoring and management.

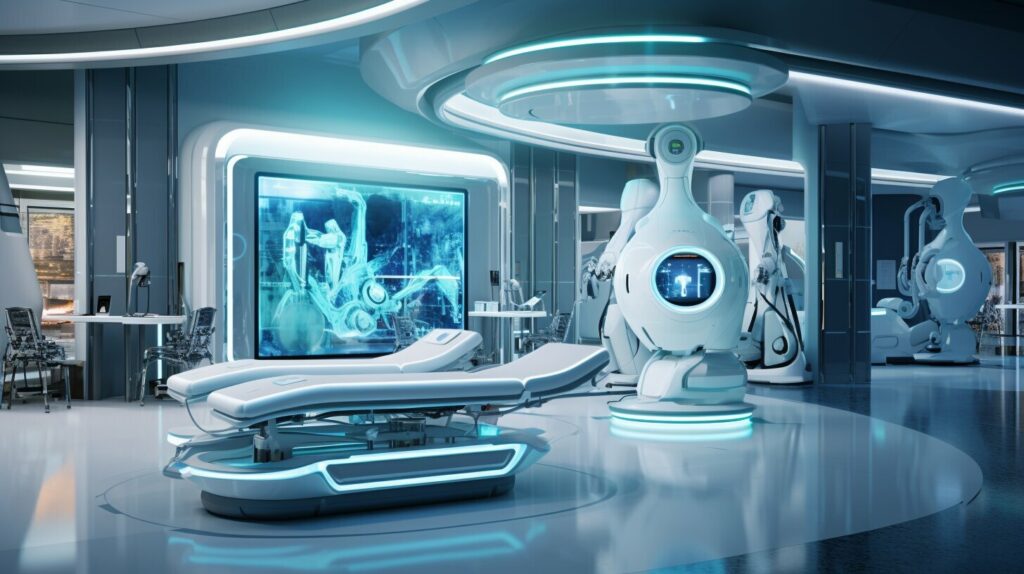
Furthermore, AI has the potential to revolutionize physician workflows in chronic disease management. By automating administrative tasks and providing support during patient visits, AI can reduce the cognitive workload of physicians and allow them to focus more on patient care. For example, AI systems can help streamline insurance requirements, summarize patient histories, and highlight key aspects for physicians. This optimization of workflows not only improves efficiency but also enhances the quality of healthcare delivery.
In conclusion, AI solutions are transforming the landscape of chronic disease management by enabling personalized interventions, accurate risk assessment, and optimized physician workflows. However, it is vital to address ethical considerations and ensure the responsible use of AI in healthcare. By leveraging the potential of AI technology, we can improve patient outcomes, reduce the burden of chronic diseases, and create a more patient-centered healthcare system.
AI’s Role in Reducing Physician Workload
As technology continues to advance, artificial intelligence (AI) is playing an increasingly significant role in the healthcare industry. One area where AI has shown great promise is in reducing the cognitive workload of physicians. By automating administrative tasks and providing support during patient visits, AI technology can optimize physician workflows, improve efficiency, and enhance the quality of healthcare delivery.
Physicians often find themselves juggling multiple tasks simultaneously, from completing insurance checklists to transcribing notes and reviewing medical records. This can be time-consuming and mentally exhausting, leaving less time for direct patient care. However, with the integration of AI systems, these administrative responsibilities can be streamlined and automated. AI can address insurance requirements, summarize patient histories, and highlight key aspects for physicians, allowing them to focus more on patient care and less on paperwork.
One significant advantage of AI in reducing physician workload is its ability to handle large volumes of data. By leveraging machine learning algorithms, AI systems can analyze vast amounts of patient information and identify patterns that may not be immediately apparent to human physicians. This not only saves time but also enhances the accuracy of diagnoses and treatment plans.
| AI’s Impact on Reducing Physician Workload | Benefits |
|---|---|
| Automating administrative tasks |
|
| Handling large volumes of data |
|
| Streamlining workflows |
|
As we look to the future, AI technology has the potential to revolutionize healthcare, transforming the physician-patient relationship. By taking care of administrative tasks and providing support, AI allows physicians to focus their expertise and attention on direct patient care, improving both efficiency and the overall healthcare experience.
While AI’s role in reducing physician workload is promising, it is crucial to strike a balance between technological efficiency and the personalized care that comes from a strong physician-patient relationship. Ensuring that AI systems are implemented ethically and responsibly will be essential in maintaining a human-centered approach to healthcare. With continued research and innovation, AI has the potential to reshape the healthcare landscape and improve patient outcomes.

AI’s Potential in Streamlining Healthcare Delivery
With the integration of AI technology, healthcare providers can optimize their workflows and streamline healthcare delivery. By automating administrative tasks, handling large volumes of data, and enhancing diagnostic accuracy, AI systems are revolutionizing the way physicians work and improving patient care.
Ethical Considerations for AI in Healthcare
As the integration of artificial intelligence (AI) in healthcare continues to advance, it is essential to address the ethical considerations that arise from this innovative technology. AI has the potential to improve patient care, enhance diagnostic accuracy, and streamline healthcare processes. However, it also presents unique challenges that must be navigated to ensure responsible and fair use.
Addressing Bias in AI
One of the primary ethical concerns with AI in healthcare is the potential for bias in algorithms and models. AI systems are developed using vast amounts of data, which may reflect bias present in the healthcare system. This can lead to inaccurate predictions or discriminatory outcomes, particularly affecting marginalized populations. To mitigate this, technologists and researchers must work towards developing equitable and transparent AI models that consider diverse populations and avoid perpetuating biases.
Ensuring Privacy and Data Security
Another crucial consideration is the protection of patient privacy and data security. AI in healthcare relies on sensitive patient information, including personal health records and medical data. It is crucial to establish robust security measures that safeguard this data from potential breaches or unauthorized access. Additionally, healthcare providers must adhere to strict privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), to ensure patient confidentiality and trust.
Establishing Ethical Guidelines
To promote the responsible and ethical use of AI in healthcare, it is essential to establish clear guidelines and standards. These guidelines should address issues such as transparency, accountability, and the responsible collection and use of data. By adhering to ethical guidelines, healthcare organizations can ensure that AI technologies are used to enhance patient outcomes while minimizing potential risks.
| Ethical Considerations for AI in Healthcare |
|---|
| Addressing Bias in AI |
| Ensuring Privacy and Data Security |
| Establishing Ethical Guidelines |

AI’s Impact on Physician-Patient Relationship
The integration of AI technology in healthcare has had a significant impact on the physician-patient relationship. On one hand, AI-powered tools and solutions have empowered patients by providing them with access to reliable healthcare information. Patients can now take an active role in their healthcare decisions, making informed choices about their treatment plans and engaging in self-care practices. This increased health literacy and patient empowerment have the potential to improve patient outcomes and overall satisfaction.
However, the reliance on AI in healthcare can also have a downside. The use of AI may create a sense of detachment or impersonality, potentially reducing the human connection between physicians and patients. The personal rapport, trust, and empathy that are integral to the physician-patient relationship may be compromised when AI assumes a greater role in patient care. It is important to strike a balance between leveraging AI for efficiency and preserving the personalized care that comes from a strong physician-patient bond.
As we continue to integrate AI into healthcare, it is crucial to prioritize the preservation and enhancement of the physician-patient relationship. This can be achieved by using AI as a tool to support and augment the care provided by physicians, rather than replacing it. AI-powered solutions can assist with administrative tasks, data analysis, and decision support, freeing up physicians’ time to focus on building relationships with their patients, providing emotional support, and addressing their unique concerns and needs.
Ultimately, the successful integration of AI in healthcare should aim to enhance the physician-patient relationship, not replace it. By leveraging AI technology responsibly and strategically, we can ensure that patients continue to receive the personalized care they need while benefiting from the advancements offered by AI in healthcare.
“The integration of AI in healthcare has the potential to empower patients, but we must remember the importance of the physician-patient relationship. In our pursuit of technological advancements, we must not lose sight of the human element in healthcare.”
The Role of Emotional Intelligence in the Age of AI
In the age of AI, emotional intelligence becomes even more crucial for healthcare professionals. While AI can assist with data analysis and decision-making, it cannot replace the human touch and empathy that physicians provide. Emotional intelligence enables physicians to connect with patients on a deeper level, understand their fears and concerns, and provide the support and reassurance needed during difficult times. By honing their emotional intelligence skills, physicians can ensure that the physician-patient relationship remains at the core of patient-centered care, even in the era of AI.
| AI’s Impact on Physician-Patient Relationship | |
|---|---|
| Positive Impacts |
|
| Negative Impacts |
|
The successful integration of AI in healthcare requires a careful consideration of its impact on the physician-patient relationship. By leveraging AI as a supportive tool and emphasizing the importance of emotional intelligence, we can maintain the human element in healthcare while harnessing the benefits offered by AI technology.
Overcoming Barriers to AI Adoption in Healthcare
AI technology has the potential to revolutionize healthcare, but several barriers hinder its widespread adoption. These barriers include the complexity of AI technology, privacy and security concerns, and the need for regulatory frameworks. Addressing these challenges is vital to ensure the responsible and effective integration of AI in healthcare.
Firstly, the complexity of AI technology poses a challenge as it requires specialized skills and resources for implementation. Healthcare organizations need to invest in training their staff and developing AI-specific expertise to fully leverage the potential of AI solutions. Overcoming this barrier involves providing education and support to healthcare professionals, enabling them to adapt to the changing landscape of healthcare.
Secondly, privacy and security concerns are significant obstacles. Healthcare data is sensitive and must be protected from potential breaches. Implementing robust security measures, utilizing encryption technologies, and adhering to strict data protection regulations are essential to build trust and ensure patient privacy in AI-driven healthcare systems.
“The integration of AI in healthcare requires the development of ethical guidelines and standards to ensure responsible and unbiased use.”
Lastly, the ethical considerations surrounding AI in healthcare must be addressed. Bias in risk assessment models and the potential lack of comprehensive and unbiased data can lead to inaccurate predictions and unfair healthcare outcomes. The integration of AI in healthcare requires the development of ethical guidelines and standards to ensure responsible and unbiased use. This involves addressing issues of algorithmic bias, transparency, and equitable access to AI-driven healthcare solutions.
Table: Barriers to AI Adoption in Healthcare
| Barrier | Description |
|---|---|
| Complexity of AI Technology | The implementation of AI requires specialized skills and resources. |
| Privacy and Security Concerns | Protecting sensitive healthcare data from breaches and ensuring patient privacy. |
| Ethical Considerations | Addressing issues of bias, transparency, and equitable access to AI-driven healthcare solutions. |
Overcoming these barriers will require collaboration between healthcare organizations, technology providers, policymakers, and regulatory bodies. By working together, we can create a future where the full potential of AI in healthcare is realized, leading to improved patient outcomes, enhanced efficiency, and transformative advancements in medical research.

Conclusion
AI solutions for healthcare, powered by healthcare artificial intelligence, are revolutionizing the industry and transforming the way medicine is practiced. These innovative technologies have the potential to enhance health literacy, improve chronic disease management, reduce physician workload, and reshape the physician-patient relationship. By leveraging the power of AI, we can create a smarter, more efficient, and more patient-centered healthcare system.
However, as we integrate AI into healthcare, we must address ethical considerations to ensure responsible and effective implementation. We need to develop equitable and transparent AI models that consider diverse populations and avoid biases. Establishing ethical guidelines and standards is crucial for the responsible use of AI in healthcare.
Additionally, there are barriers to widespread adoption that need to be overcome. The complexity of AI technology requires specialized skills and resources for implementation. Privacy and security concerns must be addressed to protect healthcare data. Regulatory frameworks need to be established to ensure ethical and responsible use. By addressing these barriers, we can pave the way for successful integration of AI in healthcare.
With continued research, collaboration, and innovation, AI solutions have the potential to reshape the future of medicine and improve patient outcomes. By embracing AI in healthcare, we can unlock new possibilities and create a healthcare system that is smarter, more efficient, and ultimately patient-centered.
FAQ
What is the role of AI in healthcare?
AI in healthcare has the potential to enhance patient care, improve health literacy, assist in chronic disease management, and transform the physician-patient relationship.
How can AI enhance health literacy?
AI can curate reliable and informative videos on health-related topics, develop gamified platforms for pediatric health literacy, and create unbiased risk assessment models to improve patients’ knowledge about managing their conditions.
How are digital vaccines using AI improving pediatric health literacy?
Digital vaccines are gamified platforms that incorporate AI-enabled immersive gaming to improve children’s knowledge about early childhood nutrition, physical activity, health-hygiene promotion, mental health, and wellness care.
How is AI being used for chronic disease management?
AI enables healthcare providers to identify high-risk patients and tailor interventions accordingly through risk assessment models that analyze comprehensive data to predict disease risks accurately.
In what ways can AI reduce the cognitive workload of physicians?
AI can automate administrative tasks, address insurance requirements, summarize patient histories, and highlight key aspects for physicians, allowing them to focus more on patient care.
What ethical challenges does the integration of AI in healthcare pose?
Potential biases in risk assessment models and the lack of comprehensive and unbiased data can result in inaccurate predictions and unfair healthcare outcomes. Ethical guidelines and standards are necessary to ensure responsible and ethical use of AI.
How does AI impact the physician-patient relationship?
AI-powered tools and solutions can empower patients by providing access to reliable information and enhancing engagement in healthcare decisions. However, reliance on AI can potentially reduce the human connection and trust between physicians and patients.
What are the barriers to widespread adoption of AI in healthcare?
The complexity of AI technology, privacy and security concerns, and the need for regulatory frameworks are significant challenges for the widespread adoption of AI in healthcare.
What is the potential of AI in healthcare?
AI has the potential to revolutionize medicine by enhancing health literacy, improving chronic disease management, reducing physician workload, and transforming the physician-patient relationship.
Bennett is the embodiment of versatility, adapting his writing to cover a broad spectrum of topics with professionalism and flair. Whether it’s breaking news, in-depth analyses, or feature pieces, Bennett’s contributions enrich Press Report with diverse perspectives and engaging content. His adaptability and keen journalistic instincts make him a vital member of our team, capable of capturing the essence of the moment in every story.

AI in Medicine
Revolutionizing Senior Living with AI Healthcare for Older Adults

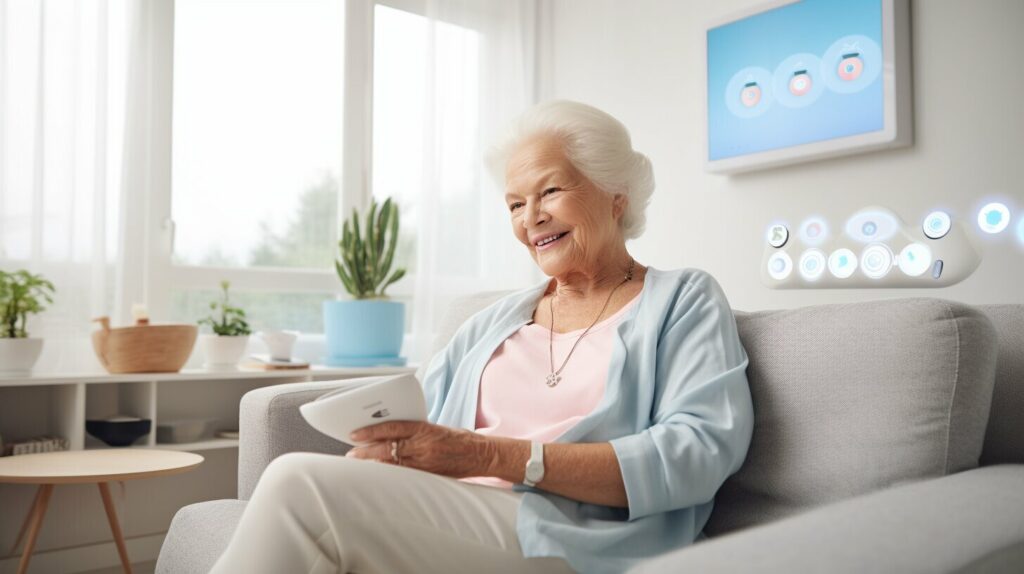
Our organization is dedicated to revolutionizing elderly care by leveraging AI healthcare for older adults. With the rising population of the elderly, it becomes crucial to explore innovative methods to meet the growing needs of this age group. Implementing AI in healthcare offers a great potential to enhance personalized care while also reducing the overall healthcare costs.
According to projections, the percentage of seniors aged 65 and above in the United States is expected to increase from 17% to 22% by 2050. This demographic shift, coupled with rising healthcare costs, necessitates a transformative approach to senior care. The average median cost of in-home care is projected to skyrocket from $4,500 to $11,000 a month by 2050, making it imperative to explore AI technology as a cost-effective solution.
AI in elder care brings a multitude of benefits, including the ability to mimic human analysis, accelerate clinical workflows, and efficiently identify health problems. This technology enables us to provide smarter, safer, and more personalized care for older adults. From AI-powered home assistants and portable devices to smart home hubs and monitoring systems, AI is reshaping the landscape of senior healthcare.
Key Takeaways:
- AI healthcare for older adults is a game-changer for the senior living industry.
- AI technology in healthcare can deliver better and more personalized care while reducing costs.
- The aging population and rising healthcare expenses necessitate innovative solutions.
- AI in elder care offers benefits such as mimicking human analysis and accelerating clinical workflows.
- AI-powered home assistants, portable devices, and smart home hubs transform the way we care for seniors.
The Benefits of AI in Elder Care
Artificial Intelligence (AI) technology has revolutionized the field of elder care, offering numerous benefits for older adults. By leveraging AI solutions, healthcare providers can deliver smarter, safer, and more personalized care, ultimately improving the quality of life for seniors.
One of the key advantages of AI in elder care is its ability to mimic human analysis and understand healthcare data. AI algorithms can quickly analyze vast amounts of medical information, helping healthcare professionals detect health problems and identify potential risks with greater efficiency.
Additionally, AI technology has the potential to significantly reduce the cost of caring for older adults. By automating certain tasks and streamlining workflows, AI systems can help mitigate the financial burden associated with elderly care. This, in turn, allows healthcare providers to allocate resources more effectively and provide better care to a larger number of seniors.
Specific applications of AI in senior healthcare include home assistants, portable devices and wearables, smart home hubs and monitoring systems, and smart implants. These technological advancements enable seniors to receive continuous care in the comfort of their own homes, while also providing healthcare professionals with real-time insights into a patient’s well-being.
The Benefits of AI in Elder Care
| Advantages | Examples |
|---|---|
| Mimics human analysis and understands healthcare data | AI algorithms can quickly analyze medical information, detect health problems, and identify risks. |
| Reduces the cost of caring for older adults | Automation and streamlined workflows help mitigate the financial burden associated with elderly care. |
| Enables continuous care at home | Home assistants, wearable devices, and monitoring systems provide real-time insights into a patient’s well-being. |
In conclusion, AI advancements in elder care have the potential to transform the way healthcare is delivered to older adults. By harnessing the power of AI technology, we can provide smarter, safer, and more personalized care, ultimately enhancing the well-being and quality of life for seniors.

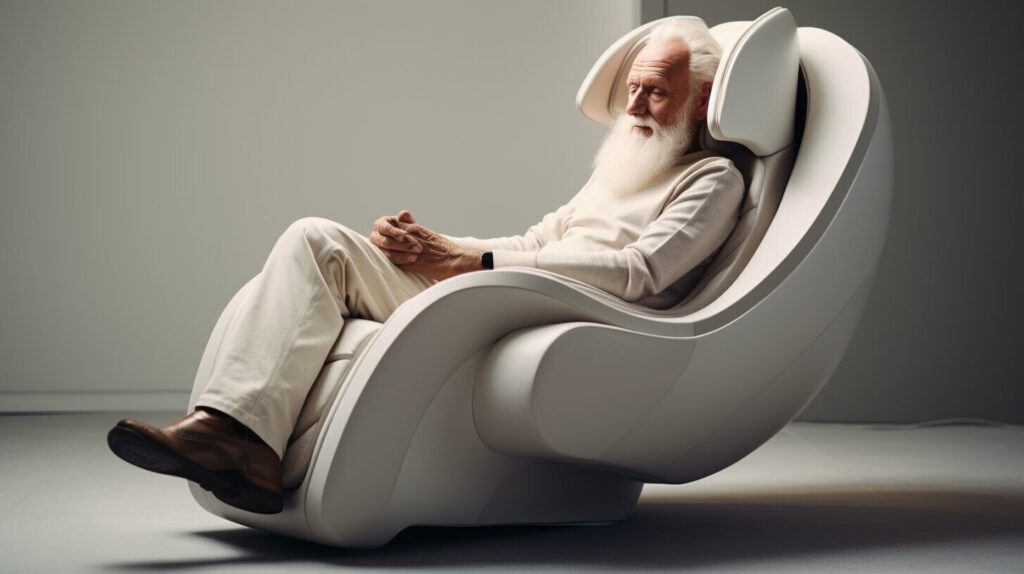
Home Assistants for Independent Living
Home assistants powered by artificial intelligence (AI) are transforming the way seniors live independently. These AI-enabled devices provide daily assistance, monitoring, and companionship for older adults who may be living alone.
One such example is the ElliQ robot. With its advanced capabilities, ElliQ engages seniors in various activities to keep them mentally stimulated and socially connected. Through video calling, seniors can stay in touch with their family and friends, reducing feelings of isolation. Additionally, home assistants like ElliQ can also serve as reminders for important tasks such as taking medications and staying hydrated.
Another AI-powered home assistant is the Mabu robot. Designed to provide personalized care and support, Mabu interacts with seniors by engaging in conversations, answering questions, and offering companionship. It can also monitor and track vital signs, reminding seniors of necessary health check-ups and appointments.
| Home Assistants for Independent Living | Features and Benefits |
|---|---|
| ElliQ robot |
|
| Mabu robot |
|
These AI-enabled home assistants are revolutionizing the way older adults can age in place. By providing support, companionship, and personalized care, these devices offer seniors greater independence and peace of mind. As the field of AI in elder care continues to evolve, home assistants will play an increasingly vital role in ensuring the well-being and quality of life for aging populations.
Portable Devices and Wearables for Health Monitoring
When it comes to senior healthcare, portable devices and wearables equipped with AI technology are revolutionizing the way we monitor and manage health. These innovative devices provide older adults with the ability to track vital signs and predict potential emergencies, empowering them to take control of their own well-being.
One such device is the Apple Watch, a popular wearable that offers a range of health monitoring features. With its built-in heart rate monitor, fall detection, and activity tracker, the Apple Watch provides seniors with real-time data to better understand their overall health and take necessary precautions.
In addition to smartwatches, companies like CarePredict have developed wearable devices specifically designed for elderly healthcare. Their Tempo Series 3 wearable uses AI algorithms to analyze data collected from the wearer, such as their activity levels, sleep patterns, and hygiene habits. This data is then used to identify any potential health issues and provide personalized recommendations for improved well-being.
By leveraging AI technology in portable devices and wearables, older adults can proactively monitor their health, detect early warning signs, and make informed decisions about their care. These devices not only promote independence and peace of mind for seniors, but also enable healthcare providers to deliver more efficient and personalized care.

Smart Home Hubs and Monitoring Systems for Safety
In the realm of AI-enabled healthcare for older adults, smart home hubs and monitoring systems play a crucial role in ensuring the safety and well-being of seniors. These innovative technologies leverage artificial intelligence to provide remote monitoring and enhance the overall care experience.
Smart home hubs, such as Alarm, utilize sensors to detect any unusual activity or changes in routine within the senior’s home. This enables caregivers or family members to receive real-time alerts and take necessary action if any concerns arise. Additionally, these systems can automatically adjust home settings, such as turning on lights or locking doors, to enhance security and provide peace of mind.
By integrating AI technology, smart home hubs and monitoring systems deliver personalized and proactive care, allowing seniors to maintain their independence while ensuring their safety. With the ability to analyze data and identify patterns, these systems have the potential to detect potential health risks or emergencies before they escalate, providing early intervention and mitigating potential harm.
The Benefits of Smart Home Hubs and Monitoring Systems for Seniors
1. Enhanced Safety: AI-powered sensors can detect unusual activities or changes in routine, allowing for immediate intervention in case of emergencies or potential risks.
2. Peace of Mind for Seniors and Caregivers: With remote monitoring capabilities, both seniors and their caregivers can have peace of mind knowing that help is readily available if needed.
3. Personalized and Proactive Care: By analyzing data and identifying patterns, smart home hubs and monitoring systems can deliver personalized care and early intervention, optimizing the overall well-being of seniors.
| Benefits | Examples |
|---|---|
| Enhanced Safety | Alarm |
| Peace of Mind | SmartThings |
| Personalized Care | Google Nest Hub |
Overall, smart home hubs and monitoring systems equipped with AI technology are revolutionizing senior healthcare by providing enhanced safety, personalized care, and peace of mind for both seniors and their caregivers. As the aging population continues to grow, these advancements in AI-assisted healthcare technology play a pivotal role in ensuring the health and well-being of older adults.
Smart Implants for Personalized Care
In the realm of AI technology in elderly care, smart implants are emerging as a game-changer, offering personalized care and real-time data for better management of health conditions. These implantable devices provide diagnostic and therapeutic benefits, improving patient outcomes and potentially reducing healthcare costs.
One remarkable example is Glysens’ implantable glucose sensor, which continuously monitors blood glucose levels for individuals with diabetes. This device eliminates the need for frequent finger pricks and allows for more accurate diabetes management. Another notable smart implant is Orthosensor’s implant in the knee, which provides detailed data on joint movement and pressure, aiding in postoperative care and recovery.
“Smart implants offer a new level of insight into patients’ health conditions, allowing for personalized and data-driven treatment plans,” says Dr. Jane Adams, a leading expert in geriatric medicine. “These devices empower both patients and healthcare professionals with the information needed to make informed decisions.”
The integration of smart implants with AI technology opens up possibilities for proactive and individualized care. By leveraging AI algorithms, these implants can analyze data in real-time, identify patterns, and provide timely alerts to healthcare providers. This enables early intervention and personalized treatment plans tailored to each patient’s unique needs.
The Potential of AI-Enabled Smart Implants
Smart implants have the potential to revolutionize the way we approach healthcare for older adults. By combining AI technology with these implantable devices, we can enhance patient monitoring, improve treatment outcomes, and promote proactive care. These advancements in personalized care not only benefit patients but also alleviate the burden on caregivers and healthcare systems.
| Smart Implant | Function |
|---|---|
| Glysens’ implantable glucose sensor | Continuous monitoring of blood glucose levels |
| Orthosensor’s implant in the knee | Detailed data on joint movement and pressure |
As AI continues to evolve and integrate with healthcare technologies, we can expect further advancements in smart implants. These innovations hold great promise for improving the quality of life for older adults and addressing the healthcare challenges associated with an aging population.
Building Trust in AI-Enabled Healthcare
In the rapidly evolving world of healthcare technology, AI has emerged as a powerful tool with the potential to revolutionize elderly care. However, to fully harness its benefits, it is crucial to build trust in AI-enabled healthcare solutions. Trust is especially vital in the healthcare industry, where the well-being and safety of seniors are at stake.
Companies like HealthEM.AI are focusing on transparency to ensure trust in AI systems. By providing care managers with the ability to understand the recommendations made by AI, these companies are demystifying the black box nature of AI algorithms. This transparency helps build confidence in the system and allows caregivers to make informed decisions based on AI-generated insights.
Transparency goes beyond simply showing the output of AI algorithms. It involves explaining the underlying processes, data sources, and the logic behind the recommendations. This thorough understanding helps caregivers and healthcare professionals overcome skepticism and adopt AI solutions with confidence. When AI systems are transparent and explainable, they become a valuable tool in augmenting human decision-making and enhancing the quality of care for older adults.
The Role of Regulation and Ethical Guidelines
Regulation and ethical guidelines also play a significant role in building trust in AI-enabled healthcare. Clear guidelines ensure that AI systems are developed, deployed, and used in an ethical manner, prioritizing patient privacy, security, and well-being. Additionally, regulation helps establish standards for data privacy and security, ensuring that sensitive health information is protected.
By adhering to these regulations and ethical guidelines, companies can demonstrate their commitment to the responsible and ethical use of AI in healthcare. This not only builds trust among caregivers and healthcare professionals but also reassures seniors and their families that their personal information and well-being are safeguarded.
Incorporating User Feedback and Collaboration
Another crucial aspect of building trust in AI-enabled healthcare is incorporating user feedback and fostering collaboration. By involving caregivers, healthcare professionals, and seniors themselves in the development and evaluation of AI solutions, companies can ensure that the technology meets their needs and addresses their concerns.
Regular feedback loops, user testing, and co-creation sessions allow stakeholders to provide input, voice concerns, and shape the development of AI-enabled healthcare. This collaborative approach not only helps build trust but also leads to the creation of more user-friendly and effective solutions.
| Benefits of Building Trust in AI-Enabled Healthcare | Examples |
|---|---|
| Increased adoption and acceptance of AI solutions | Healthcare providers embracing AI-powered remote monitoring systems for seniors |
| Improved patient outcomes and satisfaction | Seniors experiencing personalized care and proactive interventions through AI-powered wearable devices |
| Efficient and effective decision-making | Caregivers leveraging AI-powered predictive analytics to identify health risks and optimize care plans |
| Reduced healthcare costs | Healthcare organizations implementing AI-powered solutions for early detection and prevention of health issues in seniors |
Building trust in AI-enabled healthcare is a continuous process that requires collaboration, transparency, and adherence to ethical guidelines and regulations. As AI technology continues to advance, establishing trust becomes increasingly important to unlock its full potential in delivering smarter, safer, and more personalized care for older adults.
AI as a Supplement to Caregivers
AI technology is revolutionizing the field of elder care, providing innovative solutions to enhance the quality of life for older adults. However, it is important to recognize that AI should be seen as a supplement to caregivers and healthcare professionals, rather than a replacement. By working in tandem with AI tools and systems, caregivers can provide more efficient and personalized care, ultimately improving patient outcomes and experiences.
Enhancing Productivity and Quality of Care
AI tools, such as care management platforms and predictive fall risk assessment systems, can significantly enhance the productivity and quality of care provided by caregivers. Care management platforms utilize AI algorithms to analyze patient data, providing valuable insights and recommendations for personalized care plans. This enables caregivers to make more informed decisions and deliver targeted interventions, leading to better health outcomes for older adults.
Predictive fall risk assessment systems, powered by AI, can help caregivers identify and prevent falls, a common concern among seniors. These systems analyze a variety of factors, such as gait patterns and environmental conditions, to accurately predict fall risk. By leveraging this technology, caregivers can implement proactive measures to reduce fall incidents and ensure the safety of older adults, allowing them to maintain their independence for longer.
The Human Touch in Care
While AI provides valuable support and efficiency in elder care, it is essential to recognize the irreplaceable value of the human touch in caregiving. Caregivers offer emotional support, companionship, and empathy, elements that cannot be replicated by technology alone. The combination of AI technology and human caregivers creates a holistic and comprehensive approach to senior healthcare, addressing both physical and emotional needs.
By embracing AI as a supplement to caregivers, the healthcare industry can harness the full potential of technology while ensuring the delivery of compassionate and person-centered care for older adults. The collaboration between AI and caregivers is key to achieving optimal outcomes and improving the overall well-being of seniors.
| AI as a Supplement to Caregivers | Advantages |
|---|---|
| Enhanced productivity | AI tools enable caregivers to streamline workflows and make informed decisions, improving the efficiency of care delivery. |
| Personalized care | By leveraging AI algorithms, caregivers can develop tailored care plans that address the unique needs and preferences of each older adult. |
| Fall prevention | Predictive fall risk assessment systems help caregivers identify and mitigate fall risks, ensuring the safety of older adults. |
| Comprehensive approach | The combination of AI technology and human caregivers delivers a holistic approach to senior healthcare, addressing both physical and emotional needs. |
The Future of AI in Senior Healthcare
The future of healthcare technology is advancing rapidly, and AI is at the forefront of these advancements. As the population of older adults continues to grow, there is a pressing need for innovative solutions that can meet their evolving healthcare needs. AI has the potential to revolutionize senior healthcare by delivering personalized care, improving patient outcomes, and reducing healthcare costs.
One of the key use cases of AI in senior healthcare is the development of AI-powered home assistants. These intelligent robots, such as the ElliQ and Mabu robots, can provide daily assistance, monitoring, and companionship to seniors living alone. They engage seniors in activities to keep them mentally active, enable them to stay connected with loved ones through video calling, and even provide reminders for medication and hydration. These AI-powered home assistants play a crucial role in supporting independent living for older adults.
Another area where AI is making waves is in the development of portable devices and wearables for health monitoring. Devices like Apple Watches and CarePredict’s Tempo Series 3 wearable allow seniors to track their vital signs, such as heart rate and blood glucose levels. They can also detect falls through features like fall detection, providing a crucial safety net for older adults and their caregivers. These AI-enabled devices empower seniors to take control of their health and predict potential emergencies.
In addition, smart home hubs and monitoring systems are leveraging AI technology to enhance the safety and well-being of older adults. These systems use sensors to detect unusual activity or changes in routine, automatically adjusting home settings for added security. For example, the Alarm system can turn on lights or lock doors based on detected patterns. By providing remote monitoring and real-time alerts, these AI-powered systems give seniors and their caregivers peace of mind.
The future of AI in senior healthcare also includes the development of smart implants. Implants like Glysens’ glucose sensor and Orthosensor’s knee implant offer real-time data that can help manage health conditions and track postoperative care. These smart implants provide diagnostic and therapeutic benefits, improving patient outcomes and potentially reducing healthcare costs.

Summary
AI has the potential to transform the way we provide healthcare to older adults. Whether it’s through AI-powered home assistants, portable devices for health monitoring, smart home hubs, or smart implants, AI technology is paving the way for smarter, safer, and more personalized care. As the aging population continues to grow, AI will play an increasingly important role in meeting the healthcare needs of seniors, improving their quality of life, and reducing the burden on healthcare systems. The future of AI in senior healthcare is bright, offering innovative solutions for the well-being and care of older adults.
Conclusion
AI technology in senior healthcare has the potential to revolutionize the way we care for older adults. By leveraging AI-enabled solutions, we can provide smarter, safer, and more personalized care for our aging population. The use of AI in home assistants, portable devices, smart home hubs, and smart implants allows us to improve patient outcomes and address the rising costs of care.
Trust is a vital component in the successful implementation and integration of AI in senior healthcare. By focusing on transparency and collaboration between AI systems and caregivers, we can build confidence in the capabilities of AI-enabled solutions. This trust is necessary to ensure that seniors receive the best possible care and support.
The future of AI in senior healthcare looks promising. As life expectancy continues to increase and healthcare expenditures rise, AI technology provides innovative solutions to meet the growing needs of older adults. By embracing AI-enabled healthcare for older adults, we can enhance the well-being and quality of life for our seniors while driving down healthcare costs.
FAQ
What is the projected increase in the senior population in the United States?
Seniors aged 65 and above currently make up about 17% of the population in the United States, with a projected increase to 22% by 2050.
What are the benefits of AI in elder care?
AI in elder care offers numerous benefits, including the ability to mimic human analysis and understand healthcare data, speed up clinical workflows, and efficiently identify health problems.
What are some specific applications of AI in senior healthcare?
Some specific applications of AI in senior healthcare include home assistants, portable devices and wearables, smart home hubs and monitoring systems, and smart implants.
How do home assistants help seniors living alone?
Home assistants, such as the ElliQ robot and the Mabu robot, provide daily assistance, monitoring, and companionship for seniors living alone. They engage seniors in activities, keep them mentally active, allow them to stay connected with family and friends through video calling, and provide reminders for tasks like taking medications or staying hydrated.
What do portable devices and wearables for health monitoring do?
Portable devices and wearables, like Apple Watches and CarePredict’s Tempo Series 3 wearable, enable seniors to monitor their health and predict potential emergencies. These devices track vital signs, such as heart rate and blood glucose levels, and can even detect falls through features like fall detection.
How do smart home hubs and monitoring systems ensure the safety of seniors?
Smart home hubs and monitoring systems, such as Alarm, provide remote monitoring to ensure the safety and well-being of seniors. These systems use sensors to detect unusual activity or changes in routine and can automatically adjust home settings, such as turning on lights or locking doors, for added security.
What are some examples of smart implants in senior healthcare?
Examples of smart implants in senior healthcare include Glysens’ implantable glucose sensor and Orthosensor’s implant in the knee. These implants offer real-time data to help manage health conditions and track postoperative care, providing diagnostic and therapeutic benefits.
How can trust be built in AI-enabled healthcare solutions?
Trust in AI-enabled healthcare solutions can be built through transparency. Companies like HealthEM.AI focus on transparency, allowing care managers to understand the recommendations made by AI systems. The goal is to demonstrate how and why AI is functioning, ensuring trust in the system.
What is the role of AI as a supplement to caregivers?
AI tools like care management platforms and predictive fall risk assessment systems can enhance the productivity and quality of care provided by caregivers. AI should be seen as a supplement, not a replacement, to caregivers and staff members in the healthcare industry.
What is the future of AI in senior healthcare?
The future of AI in senior healthcare looks promising, offering innovative solutions for the well-being and quality of life of older adults. AI technology has the potential to revolutionize senior care, providing smarter, safer, and more personalized care while reducing healthcare costs.
In an era where technology intersects with every aspect of life, Maxwell bridges the gap between artificial intelligence and journalism. As a writer and AI expert, he explores the implications of emerging technologies on society, economy, and culture. Maxwell’s expertise allows Press Report to offer forward-thinking insights into the future of AI, making complex topics accessible and engaging for our audience.
AI in Medicine
Empowering Through Health Literacy and the Internet
Health literacy is about individuals’ ability to access, understand, and use health-related information for making informed health choices. Through the internet, there is now a wealth of online resources available to help improve their health literacy. This article seeks to explore the ways in which the internet can enhance the health literacy skills of individuals, thus empowering them.
Key Takeaways:
- The internet has revolutionized access to health information, empowering individuals to improve their health literacy.
- Digital health literacy is the ability to access, understand, and use digital health information for informed decision-making.
- Health literacy is crucial for promoting informed, healthy choices and navigating the healthcare system.
- Online health education platforms and digital health literacy tools provide valuable resources for improving health literacy skills.
- Efforts are needed to address barriers to digital health literacy, such as the digital divide and limited internet access.
The Importance of Health Literacy
Health literacy plays a vital role in promoting informed decision-making and empowering individuals to take control of their health. With the abundance of health information available online, improving health literacy through online resources has become increasingly important. Online platforms provide opportunities for health education and internet literacy, equipping individuals with the knowledge and skills needed to navigate the digital landscape of health information. By enhancing health literacy, individuals can make informed decisions about their health, effectively communicate with healthcare providers, and ultimately improve their overall well-being.
The internet offers a wealth of resources that contribute to improving health literacy. Online health education platforms provide interactive content, enabling individuals to engage with information in a way that suits their learning style. These platforms also offer comprehensive information on various health topics, ensuring individuals have access to accurate and reliable resources. By leveraging the power of the internet, individuals can expand their knowledge, gain a deeper understanding of health-related issues, and make informed choices that positively impact their health.
Internet literacy plays a significant role in health literacy by enabling individuals to navigate the vast amount of health information available online. The ability to critically evaluate and understand digital health information is essential in making informed decisions. Internet literacy skills empower individuals to distinguish between credible and unreliable sources, ensuring that they receive accurate and evidence-based information. With strong internet literacy skills, individuals can confidently navigate the web, access reliable health resources, and make informed decisions about their health and well-being.
“Improving health literacy through online resources is crucial in enabling individuals to understand and utilize health information effectively. The internet provides a vast landscape of knowledge, and by enhancing health literacy skills, individuals can harness the power of this digital platform to make informed decisions about their health.”
Health Literacy Statistics
To further emphasize the importance of health literacy, let’s take a look at some statistics:
| Statistic | Percentage |
|---|---|
| Only 12% of adults have proficient health literacy skills | 12% |
| Nearly 1 in 5 adults read at or below a fifth-grade level | 20% |
| 84% of adults have limited health literacy skills | 84% |
These statistics highlight the need for interventions and resources that can improve health literacy skills and empower individuals to make informed decisions about their health.
The Benefits of Digital Health Literacy
Digital health literacy is a valuable skillset that empowers individuals to take charge of their health and make informed decisions. The internet offers a plethora of healthcare websites and online health literacy tools that provide interactive content and easy access to reliable information. By utilizing these resources, individuals can enhance their digital health literacy skills and become more knowledgeable about their health.
One of the key benefits of digital health literacy is the ability to access healthcare websites. These websites offer a wide range of information on various health topics, from general health education to specific conditions and treatments. Users can navigate through user-friendly interfaces and explore different sections, such as symptom checkers, medication guides, and preventive care guidelines. By accessing these websites, individuals can educate themselves on health-related topics and stay informed about the latest advancements in healthcare.
Online health literacy tools are another valuable resource for promoting digital health literacy. These tools provide opportunities for self-assessment and learning, allowing individuals to test their knowledge and understanding of health information. They often offer quizzes, interactive modules, and educational materials that can help individuals improve their digital health literacy skills. By engaging with these tools, individuals can build their confidence in navigating digital health resources and making informed decisions about their health.
Promoting Health Literacy with the Internet
The internet has revolutionized the way we access and consume information, and it has the potential to greatly enhance health literacy. By utilizing healthcare websites and online health literacy tools, individuals can improve their understanding of health information, navigate the healthcare system more effectively, and ultimately make better decisions about their health. Digital health literacy is a valuable skill that empowers individuals to take control of their health and become active participants in their healthcare journey.
| Benefits of Digital Health Literacy | Examples |
|---|---|
| Access to reliable health information | Healthcare websites provide evidence-based information on a wide range of health topics |
| Interactive learning opportunities | Online health literacy tools offer quizzes, modules, and educational materials for self-assessment and learning |
| Improved decision-making | By enhancing digital health literacy skills, individuals can make informed decisions about their health |
| Empowering individuals | Digital health literacy empowers individuals to take control of their health and become active participants in their healthcare journey |
Addressing Barriers to Digital Health Literacy
Digital health literacy has the potential to greatly empower individuals in managing their health and making informed decisions. However, there are still barriers that need to be addressed to ensure equal access to digital health literacy resources. One significant barrier is the digital divide, which refers to the unequal access to technology and the internet.
The digital divide is a challenge that limits the ability of certain individuals to obtain valuable online health information and resources. Limited internet access can significantly impact an individual’s ability to improve their health literacy skills through digital platforms. Efforts need to be made to bridge this divide and provide equal access to digital health literacy tools for all individuals.
Overcoming the digital divide
To overcome the digital divide and address limited internet access, various strategies can be implemented. One approach is to increase internet accessibility in underserved areas through initiatives such as community networks or public Wi-Fi installations. Additionally, providing internet access in healthcare settings, such as clinics and hospitals, can ensure that individuals have access to online health resources when they need them.
Education and training programs are also essential in overcoming the digital divide. Teaching individuals digital literacy skills, including how to navigate the internet, evaluate online health information, and use digital health resources effectively, can empower them to overcome barriers and improve their health literacy. Collaborations between healthcare organizations, community centers, and educational institutions can help facilitate these educational initiatives.
Collaborative efforts for accessible digital health literacy
Addressing barriers to digital health literacy requires collaborative efforts between various stakeholders, including government organizations, healthcare providers, technology companies, and community groups. These collaborations can lead to the development of innovative solutions, such as mobile health applications, that can be accessed even with limited internet connectivity.
By addressing the digital divide and ensuring equal access to digital health literacy resources, we can empower individuals to become active participants in managing their health. Bridging the gap in digital health literacy will contribute to improved health outcomes and a more equitable healthcare system for all.

The Role of Patient Empowerment Network
The Patient Empowerment Network (PEN) is a nonprofit organization dedicated to empowering patients and improving health literacy. Through its innovative program, called the Digitally Empowered program, PEN aims to equip individuals with the necessary skills to navigate the digital landscape of health information. The program is accessible to anyone and provides step-by-step instructions, videos, and quizzes to enhance digital health literacy skills.
The Digitally Empowered Program
The Digitally Empowered program offered by PEN is designed to be user-friendly and accessible to individuals of all technical abilities. It consists of 10 modules that cover various topics related to digital health literacy, such as internet usage, online terminology, social media engagement, and using patient portals. Each module includes a video, a review with a resource guide, and a quiz to reinforce learning. This comprehensive program aims to equip individuals with the skills they need to navigate the digital landscape for health education and access to online health resources.

Continuing Support for Digital Health Literacy
In addition to the Digitally Empowered program, PEN provides ongoing support through its Facebook group and newsletter. These platforms allow individuals to connect with others who are also improving their digital health literacy skills, ask questions, and share their experiences. The program also offers resources for users to revisit modules, access review guides, and find answers to frequently asked questions. This continued support is crucial for individuals to reinforce their understanding and application of digital health literacy in their daily lives.
Overall, the Patient Empowerment Network and its Digitally Empowered program play a vital role in promoting health literacy and empowering individuals to take control of their own health. By equipping individuals with digital health literacy skills, PEN is helping individuals navigate the vast amount of health information available online and make informed decisions about their healthcare.
The Digitally Empowered Program
The Digitally Empowered program offered by the Patient Empowerment Network is a comprehensive online course designed to enhance individuals’ health literacy skills and promote digital health literacy. With user-friendly modules and interactive content, this program is accessible to individuals of all technical abilities, empowering them to navigate the digital landscape for health education and access online health resources.
The program consists of 10 modules that cover a range of topics essential for health technology literacy. These modules include internet usage, online terminology, social media engagement, and using patient portals. Each module features a video that provides step-by-step instructions and real-life examples, making it easier for individuals to grasp the concepts and apply them in their healthcare journeys.
To reinforce learning, every module concludes with a review and resource guide, allowing individuals to revisit the content and dive deeper into the topics that interest them. Additionally, a quiz is provided at the end of each module to test knowledge retention and provide immediate feedback. This interactive format ensures that individuals not only acquire new skills but also apply them effectively.
By participating in the Digitally Empowered program, individuals can gain the knowledge and confidence to navigate online health resources, communicate effectively with healthcare providers, and make informed decisions about their health. This program is a valuable resource for anyone seeking to improve their digital health literacy and harness the power of the internet for better health outcomes.

Table: Overview of Digitally Empowered Program Modules
| Module | Topic |
|---|---|
| Module 1 | Internet Usage for Health Education |
| Module 2 | Understanding Online Terminology |
| Module 3 | Using Social Media for Health |
| Module 4 | Navigating Healthcare Websites |
| Module 5 | Engaging with Online Support Communities |
| Module 6 | Accessing and Using Patient Portals |
| Module 7 | Understanding Health Apps and Wearables |
| Module 8 | Evaluating Online Health Information |
| Module 9 | Privacy and Security in the Digital Age |
| Module 10 | Becoming a Digital Health Advocate |
Digital Health Literacy Support: Join the Digitally Empowered Community
At the core of the Digitally Empowered program is a strong community of individuals committed to improving their digital health literacy skills. By joining the Digitally Empowered Facebook group, participants gain access to a supportive network where they can engage in discussions, ask questions, and learn from one another’s experiences. This online community serves as a valuable platform for individuals to connect, share resources, and support each other in their journey towards improved health literacy.
In addition to the Facebook group, participants can also subscribe to the Digitally Empowered newsletter. This newsletter provides regular updates on new resources, upcoming webinars, and tips for enhancing digital health literacy. Subscribers receive exclusive content that complements the program modules, helping them stay informed and motivated on their health literacy journey.
By offering ongoing support through the Facebook group and newsletter, the Digitally Empowered program ensures that individuals can continue to build on their digital health literacy skills even after completing the program. This continued support plays a crucial role in reinforcing understanding, fostering engagement, and promoting lifelong learning in the realm of health literacy.
Join the Digitally Empowered community today and take the next step towards improving your digital health literacy. Whether you’re looking to enhance your skills, connect with others, or stay updated on the latest developments in health literacy, the Digitally Empowered program has the resources and support you need to succeed.

Testimonial from a Digitally Empowered Participant:
“Joining the Digitally Empowered Facebook group and subscribing to the newsletter has been a game-changer for me. I’ve connected with like-minded individuals who understand the importance of digital health literacy, and together, we’re supporting each other’s growth. The newsletter keeps me informed and motivated, providing valuable insights and resources that complement the program modules. I highly recommend joining the Digitally Empowered community!”
The Impact of Digital Health Literacy
Digital health literacy has revolutionized the way individuals engage with their healthcare and has the potential to significantly improve health outcomes. With increased access to online resources and information, patients are empowered to take a more active role in managing their health and making informed decisions. Studies have shown that individuals with higher levels of health literacy are more likely to experience improved health outcomes and have better patient-provider relationships.
Patient engagement is a key aspect of digital health literacy, as it encourages individuals to become active participants in their healthcare journey. Through digital platforms, patients can access vital health information, communicate with healthcare providers, and join online communities for support and shared experiences. This increased engagement fosters a sense of empowerment and enables patients to make more informed decisions about their health.
Improved health outcomes are another significant impact of digital health literacy. When individuals are equipped with the skills and knowledge to navigate the digital landscape of health information, they can better understand their health conditions, treatment options, and preventive measures. By making informed decisions and proactively managing their health, patients are more likely to experience positive outcomes and lead healthier lives.
| Key Impact of Digital Health Literacy | |
|---|---|
| Patient engagement | Increased active participation in healthcare |
| Improved health outcomes | Positive impact on health management and decision-making |
Overall, digital health literacy has the power to transform the healthcare landscape by empowering individuals, improving patient-provider relationships, and promoting better health outcomes. By harnessing the benefits of the internet and increasing access to digital health resources, we can continue to enhance health literacy skills and create a more informed and engaged population.
Building Health Literacy Skills for Better Health
Improving health literacy skills is essential for individuals to make informed decisions about their health and effectively navigate the healthcare system. Health literacy interventions, such as educational programs and digital resources, play a vital role in building these skills and empowering individuals to take control of their health.
Health education programs are an effective way to enhance health literacy. These programs provide individuals with the knowledge and tools they need to understand and access reliable health information. By participating in health education courses, individuals can learn how to interpret medical terminology, navigate healthcare websites, and understand their rights as healthcare consumers.
In addition to educational programs, digital resources can also play a significant role in building health literacy. Online tools and platforms provide individuals with easy access to health information, interactive content, and self-assessment opportunities. By utilizing these digital resources, individuals can acquire essential health literacy skills and become more confident in managing their health.
Health Education Programs and Digital Resources for Health Literacy
To illustrate the impact of health education programs and digital resources on health literacy, let’s take a look at a comparative table highlighting their key features:
| Health Education Programs | Digital Resources |
|---|---|
|
|
Both health education programs and digital resources offer unique benefits in improving health literacy. While education programs provide a structured learning environment and foster group discussions, digital resources offer instant access to information and interactive learning experiences. Combining these approaches can maximize the impact of health literacy interventions and empower individuals to make informed decisions about their health.
The Global Perspective on Health Literacy
Health literacy is not only a concern within individual countries, but it is also a global issue that affects individuals in different regions of the world. Understanding health information and making informed decisions about one’s health is essential regardless of geographic location. However, the level of health literacy can vary significantly depending on a country’s resources, education systems, and cultural factors.
When considering health literacy on a global scale, it is crucial to recognize the disparities that exist. Some regions may lack access to basic health services, while others struggle with limited access to digital resources. These disparities can result in unequal health outcomes and perpetuate the cycle of health inequities.
The Importance of Addressing Health Literacy Globally
As we strive to achieve the United Nations’ Sustainable Development Goals (SDGs), addressing health literacy is essential. The SDGs aim to promote health and well-being for all, and improving health literacy aligns with this agenda. By increasing health literacy globally, we can better understand and address the social, economic, and environmental determinants of health.
“Improving health literacy globally is vital for creating a more equitable healthcare system and ensuring better health outcomes for individuals around the world.”
Efforts to improve health literacy should focus on providing accessible and culturally relevant health information in different regions. This can involve translating health materials into local languages, addressing cultural norms and beliefs, and collaborating with community leaders and organizations.
Collaboration and Knowledge Sharing
Addressing global health literacy requires collaboration and knowledge sharing among countries and organizations. By sharing best practices, strategies, and resources, we can learn from one another and develop effective approaches to improve health literacy worldwide.
Ultimately, increasing global health literacy is an investment in the well-being of individuals and communities. It empowers individuals to take control of their health, make informed decisions, and advocate for their needs in the healthcare system. By working together, we can bridge the gaps in health literacy and create a healthier, more equitable world.
| Region | Health Literacy Level |
|---|---|
| North America | High |
| Europe | High |
| Asia | Varies |
| Africa | Low |
| Latin America | Medium |
Addressing Health Inequities through Health Literacy
Health inequities continue to persist, with marginalized populations often facing higher rates of disease and poorer health outcomes. Addressing these inequities requires a multifaceted approach that includes improving health literacy among these communities. By empowering individuals with health literacy skills, we can bridge the gap and work towards reducing health disparities.
When it comes to marginalized populations, access to reliable health information and resources may be limited. This can perpetuate existing health inequities and contribute to poorer health outcomes. By focusing on health literacy, we can equip individuals with the knowledge and skills they need to advocate for their own health, navigate the healthcare system, and make informed decisions about their well-being.
A key aspect of addressing health inequities through health literacy is acknowledging and addressing the social determinants of health. These factors, such as socioeconomic status, education, and access to healthcare services, have a significant impact on an individual’s health. By promoting health literacy, we can empower individuals to understand and address these social determinants, leading to improved health outcomes for marginalized populations.
| Health Inequities | Health Literacy |
|---|---|
| – Higher disease rates | – Empowers individuals to make informed health decisions |
| – Poorer health outcomes | – Provides access to reliable health information |
| – Limited access to healthcare | – Helps navigate the healthcare system |
| – Social determinants of health | – Addresses the underlying factors impacting health |
Addressing health inequities through health literacy is a crucial step towards creating a more equitable healthcare system. By empowering marginalized populations with the knowledge and skills they need to advocate for their own health, we can begin to bridge the gap and work towards reducing disparities. It is our collective responsibility to ensure that everyone, regardless of their background, has access to the resources and tools they need to lead healthy lives.

Conclusion
In conclusion, digital health literacy is a powerful tool that empowers individuals to take control of their health and make informed decisions. The internet provides a wealth of resources and information that can enhance health literacy skills and promote better health outcomes. Initiatives like the Digitally Empowered program offered by the Patient Empowerment Network play a crucial role in promoting digital health literacy and equipping individuals with the necessary skills to navigate the digital landscape for health education.
By continuously improving health literacy, individuals can lead healthier lives, engage actively in their healthcare, and contribute to better health outcomes. Digital health literacy enables individuals to understand their health conditions, make informed decisions about treatment options, and communicate effectively with their healthcare providers. It also helps individuals address social determinants of health and advocate for their needs in the healthcare system.
Through digital health literacy, we can bridge the gap between individuals and valuable online health resources. By empowering individuals with the knowledge and tools they need, we can promote health equity and reduce health inequities among disadvantaged and marginalized populations. Ultimately, digital health literacy holds the power to transform how individuals access and utilize health information, leading to a more informed and empowered society.
FAQ
What is health literacy?
Health literacy is the ability of individuals to access, understand, and use health information to make informed decisions about their health.
How can the internet improve health literacy?
The internet provides access to a vast amount of health information and online resources that can enhance health literacy skills.
What is digital health literacy?
Digital health literacy refers to an individual’s ability to access, understand, and use digital health information to make informed decisions about their health.
What barriers exist for improving health literacy online?
The digital divide, which refers to unequal access to technology and the internet, can be a barrier to improving health literacy online.
What is the Patient Empowerment Network?
The Patient Empowerment Network is a nonprofit organization that aims to empower patients and improve health literacy.
What is the Digitally Empowered program?
The Digitally Empowered program is a free online course offered by the Patient Empowerment Network that guides individuals through the basics of digital technology and health literacy.
What topics does the Digitally Empowered program cover?
The program covers various topics such as internet usage, online terminology, social media engagement, and using patient portals.
How can individuals receive ongoing support through the Digitally Empowered program?
The program provides a Facebook group and a newsletter for individuals to connect with others and access additional resources.
How can digital health literacy impact individuals’ engagement in their healthcare?
Digital health literacy can help individuals better understand their health conditions, make informed decisions about treatment options, and communicate effectively with their healthcare providers.
What is the role of health literacy interventions?
Health literacy interventions, such as the Digitally Empowered program, can provide individuals with the knowledge and tools they need to enhance their health literacy skills.
How does health literacy align with the United Nations’ Sustainable Development Goals?
By increasing health literacy, individuals can better understand and address the social, economic, and environmental determinants of health, contributing to the achievement of the Sustainable Development Goals.
How can health literacy help reduce health inequities?
Health literacy efforts can empower individuals to advocate for their health, access reliable information, and address social determinants of health, thereby reducing health inequities.
What is the impact of digital health literacy on individuals’ health outcomes?
Studies have shown that patients with higher levels of health literacy experience improved health outcomes and have better patient-provider relationships.
How can individuals build their health literacy skills?
Building health literacy skills involves education, practice, and access to reliable resources such as health literacy interventions.
How does health literacy empower individuals?
Health literacy empowers individuals to take control of their health, make informed decisions, and advocate for their needs in the healthcare system.
In an era where technology intersects with every aspect of life, Maxwell bridges the gap between artificial intelligence and journalism. As a writer and AI expert, he explores the implications of emerging technologies on society, economy, and culture. Maxwell’s expertise allows Press Report to offer forward-thinking insights into the future of AI, making complex topics accessible and engaging for our audience.
AI in Medicine
Revolutionizing the Future: AI in Healthcare and Medicine

Dive deep with us into the revolutionary effects of artificial intelligence (AI) on healthcare and the practice of medicine. AI has the potential to utterly transform the way we manage patient care, diagnose conditions, and approach treatment options, marking the beginning of a new chapter in improved health outcomes. This article will explore the current state of AI in clinical environments, examining its role in disease detection, treatment recommendation, and enhancing patient communication, all the while addressing the challenges and ethical considerations associated with implementing AI in healthcare.
Key Takeaways:
- AI technology is reshaping healthcare by enhancing patient care and quality of life.
- AI applications in disease diagnosis are proving to be highly accurate and efficient.
- Treatment recommendations aided by AI can optimize personalized medicine options.
- AI-driven healthcare systems improve patient engagement and overall healthcare experience.
- The implementation of AI in healthcare requires responsible ethical and legal considerations.
The Growing Role of AI in Clinical Practice
Artificial intelligence (AI) is increasingly playing a vital role in clinical practice, revolutionizing healthcare and improving patient outcomes. With its ability to analyze vast amounts of data and identify patterns, AI is transforming disease diagnosis, treatment recommendations, and patient engagement.
In disease diagnosis, AI applications are proving to be highly accurate and efficient. AI systems, powered by machine learning and deep learning algorithms, can analyze medical images and detect abnormalities with greater precision than human physicians. For example, in cancer diagnosis, AI algorithms have demonstrated high sensitivity and specificity, leading to early detection and more effective treatment plans.
When it comes to treatment recommendations, AI can provide personalized options based on patient data and medical literature. By considering patients’ specific characteristics, AI algorithms can predict treatment outcomes and help healthcare professionals make informed decisions. AI also contributes to drug discovery, analyzing vast datasets to identify potential medications for various diseases.
| AI Applications in Clinical Practice | Benefits |
|---|---|
| Disease Diagnosis | Improved accuracy and early detection |
| Treatment Recommendations | Personalized medicine and optimized treatment plans |
| Patient Engagement | Enhanced communication and education |
Furthermore, AI is enhancing patient engagement and care. AI-driven systems can provide virtual health assistants, offering round-the-clock support and guidance to patients. These assistants can answer questions, provide educational resources, and monitor patients’ health status remotely. By empowering patients with information and personalized care, AI is revolutionizing the healthcare experience.
As AI continues to advance, it is crucial to address the ethical and legal considerations surrounding its implementation. Data privacy, algorithm biases, and the need for human expertise are among the challenges that need to be addressed for the responsible use of AI in healthcare. By navigating these challenges, we can unlock the full potential of AI and shape the future of clinical practice.

The Future of AI in Clinical Practice
The future of AI in clinical practice holds great promise. Ongoing research and development are expected to further improve AI’s capabilities in disease diagnosis, treatment recommendations, and patient care. As AI technologies continue to evolve, healthcare professionals and patients alike can look forward to a future where AI plays a central role in delivering high-quality, personalized healthcare.
AI in Disease Diagnosis
AI technology is making significant strides in the field of disease diagnosis. With the ability to analyze large datasets and utilize advanced algorithms, AI tools are proving to be invaluable in accurately detecting and diagnosing various medical conditions. These advancements have the potential to revolutionize healthcare by improving diagnostic accuracy and facilitating early intervention.
One area where AI has shown great promise is in cancer diagnosis. Studies have shown that AI systems can effectively detect breast cancer and skin cancer, often surpassing the accuracy of human physicians. By analyzing vast amounts of medical imagery and utilizing deep learning techniques, AI algorithms can identify subtle patterns and early-stage indicators of cancer, enabling timely diagnosis and treatment.
AI in disease diagnosis has the potential to transform healthcare by improving accuracy and enabling early intervention.
In addition to cancer, AI is also being utilized in dermatology diagnosis. Skin conditions can be challenging to diagnose accurately, especially for rare or complex diseases. However, AI algorithms can analyze images of skin conditions and compare them with extensive databases to provide accurate and efficient diagnoses. This aids dermatologists in providing appropriate treatment options and improving patient outcomes.
AI Tools for Disease Diagnosis
Various AI tools are being developed for disease diagnosis, including computer-aided detection (CAD) systems and AI-powered medical imaging technologies. CAD systems use algorithms to analyze medical images, assisting radiologists in detecting abnormalities and making accurate diagnoses. Similarly, AI-powered medical imaging technologies can analyze complex medical images, such as X-rays and MRIs, to aid in the diagnosis of various conditions.
The table below provides an overview of AI advancements in disease diagnosis:
| Disease | AI Application | Benefits |
|---|---|---|
| Breast Cancer | AI-powered mammography analysis | Improved accuracy in detecting early-stage cancer |
| Skin Cancer | AI analysis of dermoscopy images | Accurate and efficient diagnosis of skin conditions |
| Lung Cancer | Computer-aided detection systems for chest X-rays | Enhanced detection of early-stage lung cancer |
These advancements in AI for disease diagnosis have the potential to revolutionize healthcare by improving accuracy, facilitating early intervention, and ultimately saving lives. As AI continues to evolve, it is crucial for healthcare professionals and researchers to collaborate and harness the full potential of this technology in the fight against various diseases.

AI in Treatment Recommendations
AI has emerged as a valuable tool in providing treatment recommendations, offering personalized medicine options, and aiding in drug discovery. With its ability to analyze vast amounts of patient data, AI can assist healthcare professionals in making informed decisions and optimizing treatment outcomes.
One of the significant advantages of AI in treatment recommendations is the ability to provide personalized medicine options. By leveraging machine learning algorithms, AI can analyze individual patient data, including medical history, genetics, lifestyle factors, and treatment responses. This analysis enables AI to generate tailored treatment plans that consider unique patient characteristics, ultimately improving treatment efficacy.
AI is also making significant contributions to the field of drug discovery. Through advanced algorithms and data mining techniques, AI can identify potential therapeutic targets and predict the effectiveness of experimental treatments. This capability accelerates the drug discovery process, reducing costs and time to market, and potentially leading to the development of more effective treatments for various diseases.
Additionally, AI technology aids in treatment selection by predicting treatment outcomes and optimizing medication dosages. By analyzing large datasets and learning from patterns in patient responses, AI algorithms can provide healthcare professionals with valuable insights and recommendations. This support empowers physicians to make more informed decisions and potentially improve patient outcomes.
| Advantages of AI in Treatment Recommendations | Applications |
|---|---|
| Personalized medicine | Using patient data to generate tailored treatment plans |
| Drug discovery | Identifying potential therapeutic targets and predicting treatment effectiveness |
| Treatment selection | Predicting treatment outcomes and optimizing medication dosages |
AI in treatment recommendations enables healthcare professionals to provide personalized and optimized care, improving treatment efficacy and patient outcomes.
In conclusion, AI plays a crucial role in treatment recommendations by providing personalized medicine options, aiding in drug discovery, and optimizing treatment selection. The ability of AI to analyze vast amounts of patient data and identify patterns allows for more informed decision-making and potentially improved patient outcomes. As AI technology continues to advance, its contributions to treatment recommendations are expected to further enhance the field of healthcare.

AI in Patient Engagement and Care

AI is playing an increasingly important role in patient engagement and care, revolutionizing the way healthcare is delivered. With the development of AI-driven healthcare systems, patients can now benefit from personalized recommendations and improved access to information and support.
One of the key applications of AI in patient engagement is through the use of virtual health assistants. These AI-powered tools can provide personalized guidance, answer questions, and offer support to patients, enhancing their overall healthcare experience. Virtual health assistants can also help with patient education, providing detailed explanations of medical conditions, treatment options, and medication instructions.
AI-driven healthcare systems have the potential to greatly improve patient care and outcomes. With virtual health assistants and personalized recommendations, patients can have a more active role in their healthcare journey.
In addition to virtual health assistants, AI can also support mental health care by analyzing patient data and identifying potential issues. Through sentiment analysis and natural language processing, AI algorithms can detect changes in mood and behavior, alerting healthcare professionals to intervene and provide timely support.
By leveraging AI in patient engagement and care, healthcare providers can enhance the patient experience, improve health outcomes, and empower individuals to take a more proactive approach to their own well-being.
AI in Patient Engagement and Care Summary:
- AI-powered virtual health assistants provide personalized guidance and support to patients.
- AI can enhance patient education by providing detailed explanations and information.
- AI supports mental health care by analyzing patient data for early detection of issues.
- By leveraging AI, healthcare providers can improve the patient experience and empower individuals in their own healthcare journey.
Table: Benefits of AI in Patient Engagement and Care
| Benefits | Description |
|---|---|
| Personalized Recommendations | AI-driven systems offer personalized treatment and care suggestions based on patient data. |
| Improved Access to Information | Virtual health assistants provide instant access to medical information and resources. |
| Enhanced Patient Education | AI tools offer detailed explanations and education materials for patients to better understand their conditions and treatments. |
| Support for Mental Health Care | AI algorithms can analyze patient data to detect changes in mood and behavior, enabling early intervention and support. |
With AI-driven healthcare systems and virtual health assistants, the future of patient engagement and care looks promising. As technology continues to advance, we can expect further innovations and improvements in healthcare delivery, ultimately leading to better patient outcomes and a more patient-centered approach to care.
Ethical and Legal Considerations in AI Implementation
As we delve into the world of AI in healthcare, it is crucial to address the ethical and legal considerations associated with its implementation. While AI holds immense potential for improving patient care and outcomes, responsible use and adherence to ethical guidelines are paramount. We must navigate the complex landscape of data privacy, biases in AI algorithms, and the need for human expertise to ensure the responsible implementation of AI in healthcare.
One of the key ethical considerations is data privacy. As AI algorithms analyze vast amounts of patient data, it is essential to protect individuals’ privacy and ensure that sensitive information is secure. Striking a balance between deriving valuable insights from data and safeguarding patient privacy is crucial for building trust in AI-driven healthcare systems. The responsible handling of data can help mitigate concerns regarding data breaches and misuse of personal health information.
Another important consideration is the potential biases that may exist within AI algorithms. AI systems learn from large datasets, and if these datasets contain biases, it can inadvertently perpetuate those biases in healthcare decision-making. Recognizing and addressing these biases is essential to ensure fair and equitable treatment for all patients. Regular audits and algorithmic transparency can help identify and rectify biases, promoting fairness and equality in healthcare delivery.
AI in healthcare must be implemented with careful consideration and adherence to legal frameworks. Compliance with existing regulations, such as HIPAA in the United States, is essential to protect patient confidentiality and ensure the responsible use of AI. Additionally, as AI continues to evolve, it is important to stay updated on legal developments and adapt AI systems accordingly. This can help mitigate legal risks and ensure that AI is utilized in a manner that aligns with legal requirements and patient rights.
Responsible implementation of AI in healthcare
In order to ensure the responsible implementation of AI in healthcare, collaboration between healthcare professionals, policymakers, and technology experts is necessary. Multidisciplinary discussions can help establish guidelines and frameworks that address the ethical and legal considerations associated with AI. Furthermore, ongoing monitoring and evaluation of AI systems are crucial to detect and rectify any ethical or legal issues that may arise.
By taking a proactive approach to address ethical and legal considerations, we can harness the power of AI to improve patient care while upholding the highest standards of ethics and privacy. Responsible AI implementation in healthcare holds the promise of revolutionizing the field and transforming the way we deliver quality care to patients.

| Ethical Considerations | Legal Considerations |
|---|---|
| Data privacy | Compliance with regulations (e.g., HIPAA) |
| Biases in AI algorithms | Staying updated on legal developments |
| Ensuring fairness and equality |
The Future of AI in Healthcare
As we continue to push the boundaries of technological innovation, the future of AI in healthcare holds immense promise for transforming the field of medicine. With ongoing advancements and breakthroughs, AI technology is poised to revolutionize patient care, diagnostics, and treatment. The potential impact of AI in healthcare is vast, with the ability to improve accuracy, efficiency, and accessibility.
AI advancements in medicine are enabling us to harness the power of large datasets and complex algorithms to diagnose diseases with greater precision and speed. By analyzing vast amounts of patient data, AI can identify patterns and detect early stages of diseases, leading to earlier intervention and improved outcomes. This has the potential to revolutionize disease diagnosis and improve healthcare outcomes for patients.
Additionally, AI technology in healthcare is paving the way for personalized medicine. AI algorithms can analyze patient data, including genetic information, to recommend treatment options tailored to an individual’s unique characteristics. By optimizing treatment recommendations, AI has the potential to improve patient outcomes and enhance the effectiveness of therapies.
| AI Advancements in Medicine | AI Technology in Healthcare |
|---|---|
| Improved disease diagnosis | Predictive analytics |
| Personalized treatment recommendations | Virtual health assistants |
| Enhanced patient care | Workflow automation |
While AI in healthcare presents exciting opportunities, it is crucial to address ethical considerations and navigate potential challenges. As AI becomes increasingly integrated into healthcare systems, it is important to ensure data privacy, minimize biases in algorithms, and preserve the human element in patient care. Responsible implementation and ongoing ethical discussions will be essential to maximize the benefits of AI in healthcare.
As we look to the future, the potential of AI in healthcare is both exhilarating and transformative. With ongoing research and development, AI technologies will continue to evolve and have a significant impact on the field of medicine. The future is bright, and we are excited to be part of this journey towards leveraging AI to revolutionize healthcare and improve patient outcomes.
The Challenges and Limitations of AI in Healthcare
Implementing artificial intelligence (AI) in healthcare comes with its own set of challenges and limitations. While AI has the potential to revolutionize patient care and improve healthcare outcomes, it is important to address these hurdles for responsible and effective implementation.
One of the main challenges is ensuring data privacy and security. As AI relies on vast amounts of patient data, it is crucial to protect sensitive information and adhere to strict privacy regulations. Healthcare organizations must implement robust security measures to safeguard patient data and prevent unauthorized access.
Bias in AI algorithms is another significant concern. AI systems learn from data, and if the data is biased or incomplete, it can lead to biased outcomes. To mitigate this, it is essential to have diverse and representative datasets that account for different demographics. Additionally, ongoing monitoring and evaluation of AI systems can help identify and rectify any biases that may arise.
Another limitation of AI in healthcare is the need for human expertise. While AI can assist in diagnosing diseases and recommending treatments, it cannot replace the knowledge and experience of healthcare professionals. Combining the strengths of AI with human expertise can lead to more accurate diagnoses and better patient outcomes. Therefore, it is crucial to strike a balance between AI technologies and human intervention.
In summary, the challenges and limitations of AI in healthcare include data privacy, bias in algorithms, and the need for human expertise. Addressing these issues is essential for responsible and effective implementation of AI in clinical practice. By overcoming these hurdles, we can harness the full potential of AI to revolutionize healthcare and improve patient care.
AI for Healthcare Professionals
AI is revolutionizing healthcare by providing valuable support to healthcare professionals in their roles. Rather than replacing physicians, AI technology complements their expertise, assisting with accurate diagnoses, treatment recommendations, and workflow management. As the field of healthcare evolves, so do the roles of physicians in an AI-driven healthcare system.
AI training for physicians is becoming increasingly important to ensure they can effectively leverage AI technology in their practice. By mastering AI tools and algorithms, healthcare professionals can enhance their decision-making processes and improve patient outcomes. This training equips physicians with the skills necessary to interpret and utilize AI-generated data, enabling them to deliver more precise and personalized care.
The Impact of AI on the Healthcare Workforce
The integration of AI in healthcare introduces new possibilities for the healthcare workforce. While some fear that AI may replace healthcare professionals, it is more likely that AI will reshape their roles. As AI takes on routine and time-consuming tasks, physicians can focus more on complex patient care and decision-making, resulting in improved efficiency and patient satisfaction.
Additionally, AI technology can help address the growing demand for healthcare services by reducing workloads and enhancing productivity. With AI-powered tools, healthcare professionals can streamline administrative tasks, optimize scheduling, and improve patient flow. This enables healthcare providers to see more patients, ultimately increasing access to quality care.
Overall, AI is transforming healthcare by empowering healthcare professionals with advanced tools and capabilities. By embracing AI training and adopting AI-driven healthcare systems, physicians can enhance their practice, improve patient outcomes, and shape the future of healthcare.
Conclusion
In conclusion, AI is revolutionizing healthcare and medicine by transforming patient care, diagnostics, and treatment. The advancements in AI technology are paving the way for improved healthcare outcomes and a more efficient healthcare system. With the ability to analyze large datasets and identify patterns, AI has the potential to assist healthcare professionals in disease diagnosis, treatment recommendations, and patient engagement.
However, the implementation of AI in healthcare comes with ethical and legal considerations that must be addressed for responsible use. Issues such as data privacy and biases in AI algorithms require careful attention to ensure patient safety and trust. Additionally, challenges and limitations such as the need for human expertise must be overcome to maximize the benefits of AI in healthcare.
Looking ahead, the future of AI in medicine is promising. Ongoing research and development will continue to enhance AI technologies, leading to further advancements and innovations in disease diagnosis, treatment, and patient care. We must embrace the transformative power of AI in healthcare and work towards responsible and effective implementation, ensuring that AI complements the expertise of healthcare professionals and improves the overall quality of healthcare.
FAQ
How can AI revolutionize healthcare?
AI can revolutionize healthcare by assisting with disease diagnosis, recommending treatment options, and improving patient engagement. AI technologies analyze large datasets and identify patterns that surpass human performance in healthcare tasks.
What are the applications of AI in clinical practice?
AI is being utilized for disease diagnosis, treatment recommendations, and patient engagement. It can accurately diagnose diseases like cancer and dermatology conditions, predict treatment outcomes, and provide personalized medicine options. AI-driven healthcare systems can also support patient education and provide virtual health assistants.
How accurate is AI in disease diagnosis?
Studies have shown that AI systems can accurately diagnose diseases such as breast cancer and skin cancer, often outperforming human physicians. By analyzing large datasets and using deep learning techniques, AI can identify patterns and detect early stages of diseases.
What is the role of AI in treatment recommendations?
AI can assist healthcare professionals in making treatment recommendations by analyzing patient data and providing personalized medicine options. Through machine learning algorithms, AI can predict treatment outcomes and optimize medication dosages. AI is also being used in drug discovery to identify potential treatments for various diseases.
How can AI enhance patient engagement and care?
AI-driven healthcare systems can provide virtual health assistants, support mental health care, and improve patient education. These systems automate tasks, provide personalized recommendations, and improve patient-physician trust, thereby enhancing patient engagement and care.
What are the ethical and legal considerations in AI implementation?
The implementation of AI in healthcare raises ethical and legal considerations that must be addressed. Issues such as data privacy, biases in AI algorithms, and the need for human expertise must be carefully considered for responsible and effective use.
What does the future hold for AI in healthcare?
The future of AI in healthcare holds great potential for further advancements and innovations. Ongoing research and development are expected to continue improving disease diagnosis, treatment recommendations, and patient care.
What are the challenges and limitations of AI in healthcare?
While AI offers numerous benefits in healthcare, there are also challenges and limitations that need to be addressed. Issues such as data privacy, biases, and the need for human expertise can impact the responsible and effective implementation of AI in healthcare settings.
How can AI support healthcare professionals?
AI can support healthcare professionals by providing accurate diagnoses, treatment recommendations, and workflow management. It can assist physicians in their roles, but it is not meant to replace them. AI technology can enhance healthcare outcomes by augmenting human expertise.
How is AI transforming the future of healthcare?
AI is transforming the future of healthcare by revolutionizing patient care, diagnostics, and treatment. From disease diagnosis to treatment recommendations and patient engagement, AI technologies have the potential to improve healthcare outcomes.
In an era where technology intersects with every aspect of life, Maxwell bridges the gap between artificial intelligence and journalism. As a writer and AI expert, he explores the implications of emerging technologies on society, economy, and culture. Maxwell’s expertise allows Press Report to offer forward-thinking insights into the future of AI, making complex topics accessible and engaging for our audience.
-

 AI Entertainment1 month ago
AI Entertainment1 month agoOpenAI Releases SORA: Breakthrough AI Platform
-

 AI in Legal6 days ago
AI in Legal6 days agoRevolutionizing Justice: How AI is Transforming the Legal Landscape
-

 AI in Business6 days ago
AI in Business6 days agoAI: The Powerhouse Driving Tomorrow’s Industries
-

 AI in Business4 days ago
AI in Business4 days agoSecure Your Future with AI Data Privacy Assurance
-

 AI in Legal6 days ago
AI in Legal6 days agoFrom Briefs to Bytes: The Impact of AI on Legal Documentation
-

 AI in Medicine3 days ago
AI in Medicine3 days agoRevolutionizing the Future: AI in Healthcare and Medicine
-

 AI in Medicine2 days ago
AI in Medicine2 days agoRevolutionizing Senior Living with AI Healthcare for Older Adults
-

 AI Security4 days ago
AI Security4 days agoUnlock the Power of Robust AI Security for Your Business











